Introduction: Cardiac arrhythmias can be among the most challenging conditions to treat, especially when patients suffer from recurrent shocks from an Automated Implantable Cardioverter Defibrillator (AICD). The shock, while potentially lifesaving, can be a reminder of the heart’s precarious condition, and for many, this cycle of shocks can be physically and emotionally draining. For patients whose arrhythmias persist despite extensive ablation therapies and anti-arrhythmic medications, the treatment options are limited, and a new solution becomes essential.
In this case study, we explore the successful use of bilateral thoracoscopic sympathectomy to manage recurrent AICD shocks in a patient. This procedure, often considered a last resort, provided the patient with complete relief from AICD shocks after an extensive three-month follow-up period. In this blog, we will detail the procedure, its potential benefits, and why it stands out as a breakthrough approach for patients struggling with difficult-to-treat arrhythmias.
Understanding the Challenges of Recurrent AICD Shocks:
An AICD, also known as an implantable cardioverter-defibrillator, is a medical device used to monitor and correct life-threatening arrhythmias in patients with a history of sudden cardiac arrest or severe ventricular arrhythmias. The AICD delivers a shock to the heart when it detects abnormal rhythms that could lead to life-threatening situations. However, recurrent AICD shocks, while necessary in some cases, can be damaging, both physically and emotionally for patients. These shocks often indicate that the arrhythmia is not being adequately controlled by the standard therapies.
In many instances, patients who experience frequent shocks despite undergoing comprehensive treatment, including endocardial and epicardial ablations (procedures that aim to destroy tissue causing the arrhythmias) and taking optimal anti-arrhythmic medications, are faced with a frustrating lack of options. This is where bilateral thoracoscopic sympathectomy may offer a new avenue for relief.
What is Bilateral Thoracoscopic Sympathectomy?
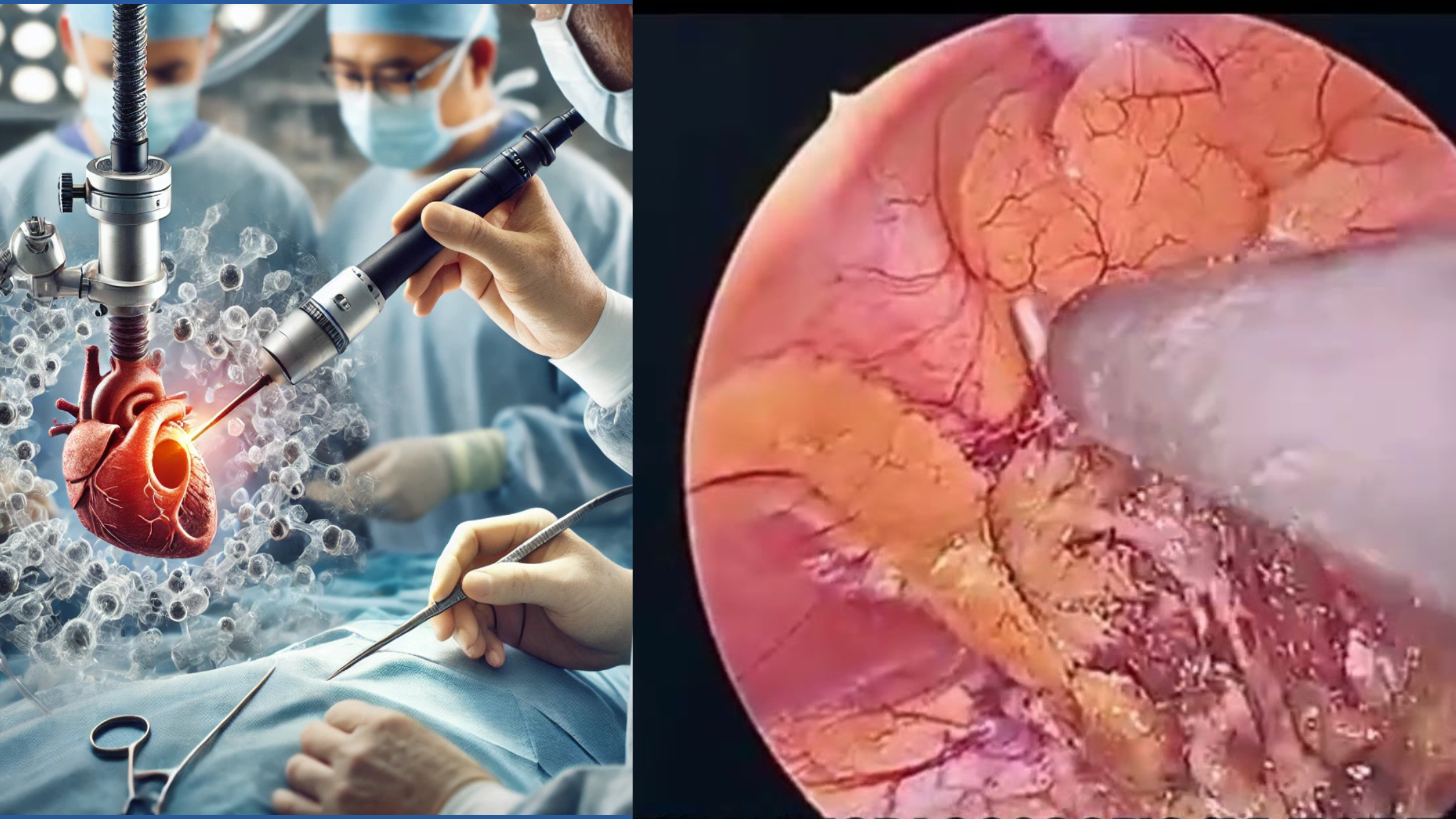
Bilateral thoracoscopic sympathectomy is a minimally invasive surgical procedure aimed at removing or interrupting the sympathetic nerves that are believed to contribute to arrhythmic activity. This procedure is performed using a thoracoscope, a small camera inserted through tiny incisions in the chest, making it a less invasive option compared to traditional open surgeries. The goal is to interrupt the sympathetic pathways that can trigger or exacerbate arrhythmias, particularly in cases where traditional treatments have failed.
Sympathectomy targets the sympathetic nerves located near the heart, which are often involved in regulating the heart’s rhythm. By severing or blocking these nerves, the procedure can help stabilize the heart’s electrical activity, potentially reducing the incidence of recurrent arrhythmias and, consequently, the need for AICD shocks.
The Procedure:
In this case study, the patient had undergone extensive endocardial and epicardial ablation procedures as well as being on the most appropriate anti-arrhythmic medications. Despite these interventions, the patient continued to experience recurrent AICD shocks. After evaluating all treatment options, it was decided that bilateral thoracoscopic sympathectomy could provide the patient with the best chance for relief.
The procedure was performed by a skilled surgical team under the leadership of Dr. Manjunath B, whose expertise in thoracic surgery ensured that the intervention was as effective as possible. The steps of the procedure included:
-
Anesthesia and Positioning: The patient was placed under general anesthesia and positioned to allow access to the chest cavity through small incisions, typically around the sides of the chest.
-
Insertion of the Thoracoscope: A thoracoscope (a small, flexible tube with a camera) was inserted into the chest to provide a clear view of the heart and the sympathetic nerves.
-
Identification and Disruption of Sympathetic Nerves: The surgeon identified the sympathetic nerve pathways near the heart and severed or interrupted them to prevent them from transmitting signals that might trigger arrhythmias.
-
Minimally Invasive Techniques: The procedure was performed using a minimally invasive technique, which reduced the risk of complications and shortened recovery time. The thoracoscopic approach allowed for smaller incisions, resulting in less trauma to the body and a quicker recovery period.
-
Post-Procedure Care and Follow-Up: Following the procedure, the patient was monitored closely for signs of improvement and possible complications. The initial post-operative period was uneventful, and the patient was discharged after a short stay in the hospital.
The Outcome:
Following the bilateral thoracoscopic sympathectomy, the patient was monitored over a three-month period. Remarkably, the patient experienced complete relief from AICD shocks. The heart’s rhythm stabilized, and the patient was no longer subjected to the distressing experience of receiving shocks from the device.
The patient reported feeling completely asymptomatic post-procedure, and there was no recurrence of the arrhythmia that had previously triggered the shocks. This outcome was a major success, considering the patient’s prior history of refractory arrhythmias and their lack of response to traditional therapies.
Why This Procedure Is Groundbreaking:
Bilateral thoracoscopic sympathectomy has been used in a variety of settings, but its use in the context of recurrent AICD shocks is relatively novel. This procedure offers several potential advantages over more traditional treatments for arrhythmias, particularly for patients who have not responded to ablation or medication.
-
Minimally Invasive: Unlike open-chest surgery, which requires large incisions and significant recovery time, bilateral thoracoscopic sympathectomy is minimally invasive, requiring only small incisions and offering quicker recovery times for patients.
-
Long-Term Relief: As evidenced in this case, the procedure offers long-term relief from arrhythmias and AICD shocks. The patient was able to live without further interventions for three months after the surgery, a period of stability that would have been difficult to achieve with other therapies.
-
Alternative to More Aggressive Treatments: For patients who do not respond to medication or ablation, or who cannot tolerate the side effects of these treatments, this procedure presents a viable alternative with potentially fewer risks and complications.
-
Improved Quality of Life: Recurrent AICD shocks can be incredibly distressing, both physically and emotionally. By eliminating the need for shocks, bilateral thoracoscopic sympathectomy can significantly improve the patient’s quality of life, reducing the stress and anxiety associated with frequent device activation.
Post-Procedure Care and Recovery:
After undergoing the procedure, the patient was provided with detailed instructions for post-operative care. This included regular follow-ups to monitor the heart’s rhythm and ensure there were no signs of complications. Patients undergoing this procedure typically experience a faster recovery than those who undergo traditional open-chest surgery, with many returning to normal activities within a few weeks.
In this case, the patient’s three-month follow-up showed no recurrence of arrhythmia, and they reported feeling completely asymptomatic. This marks a significant improvement in the patient’s condition, and it suggests that bilateral thoracoscopic sympathectomy could become an increasingly important tool in the treatment of refractory arrhythmias.
FAQs
1. What is bilateral thoracoscopic sympathectomy? Bilateral thoracoscopic sympathectomy is a minimally invasive surgical procedure aimed at interrupting the sympathetic nerve pathways that can trigger arrhythmias. It involves making small incisions in the chest and using a thoracoscope to view and sever or block these nerves.
2. How does bilateral thoracoscopic sympathectomy help with recurrent AICD shocks? The procedure helps by targeting the sympathetic nerves involved in arrhythmias, thereby reducing the incidence of abnormal heart rhythms that trigger AICD shocks. This can provide long-term relief from arrhythmias, as demonstrated in this case study.
3. Is bilateral thoracoscopic sympathectomy a safe procedure? Yes, it is considered safe when performed by an experienced surgical team. The procedure is minimally invasive, which reduces the risk of complications and promotes faster recovery.
4. How long does it take to recover from bilateral thoracoscopic sympathectomy? Most patients experience a quicker recovery compared to traditional open-heart surgery. Recovery time can vary, but many patients return to normal activities within a few weeks.
5. Are there any risks associated with bilateral thoracoscopic sympathectomy? As with any surgery, there are risks, including infection, bleeding, and complications related to anesthesia. However, the procedure is generally considered safe and well-tolerated.
6. Can bilateral thoracoscopic sympathectomy be used for all patients with recurrent AICD shocks? No, this procedure is typically considered for patients who have not responded to other treatments, including medications and ablation. A thorough evaluation by a heart specialist is necessary to determine if it is appropriate for a specific patient.
7. How successful is bilateral thoracoscopic sympathectomy in preventing AICD shocks? In this case study, the patient experienced complete relief from AICD shocks for three months following the procedure. While success rates can vary, this case demonstrates the potential of the procedure in offering long-term relief for patients with refractory arrhythmias.