When your heart skips a beat during a romantic movie, that’s sweet.
When it skips a beat while you’re quietly sitting at home — that’s a warning sign.
For millions worldwide, those skipped beats, rapid pulses, and irregular rhythms are due to atrial fibrillation (AF) — the most common sustained heart rhythm disorder.
And here’s the real danger: AF isn’t just an inconvenience; it’s a major risk factor for stroke, heart failure, and even sudden cardiac death.
Thankfully, modern heart rhythm care has moved beyond just medications. One groundbreaking option is Cryoablation — a minimally invasive procedure that literally freezes AF in its tracks.
Understanding Atrial Fibrillation
AF happens when the atria (upper heart chambers) beat chaotically instead of rhythmically.
This electrical chaos disrupts normal pumping, causes symptoms like palpitations and fatigue, and increases the risk of clots forming in the heart.
Common symptoms:
-
Fluttering or pounding heartbeat
-
Shortness of breath
-
Fatigue
-
Dizziness
-
Reduced exercise tolerance
Major risk: Blood clots from the quivering atria can travel to the brain and cause a stroke — AF increases stroke risk by five times.
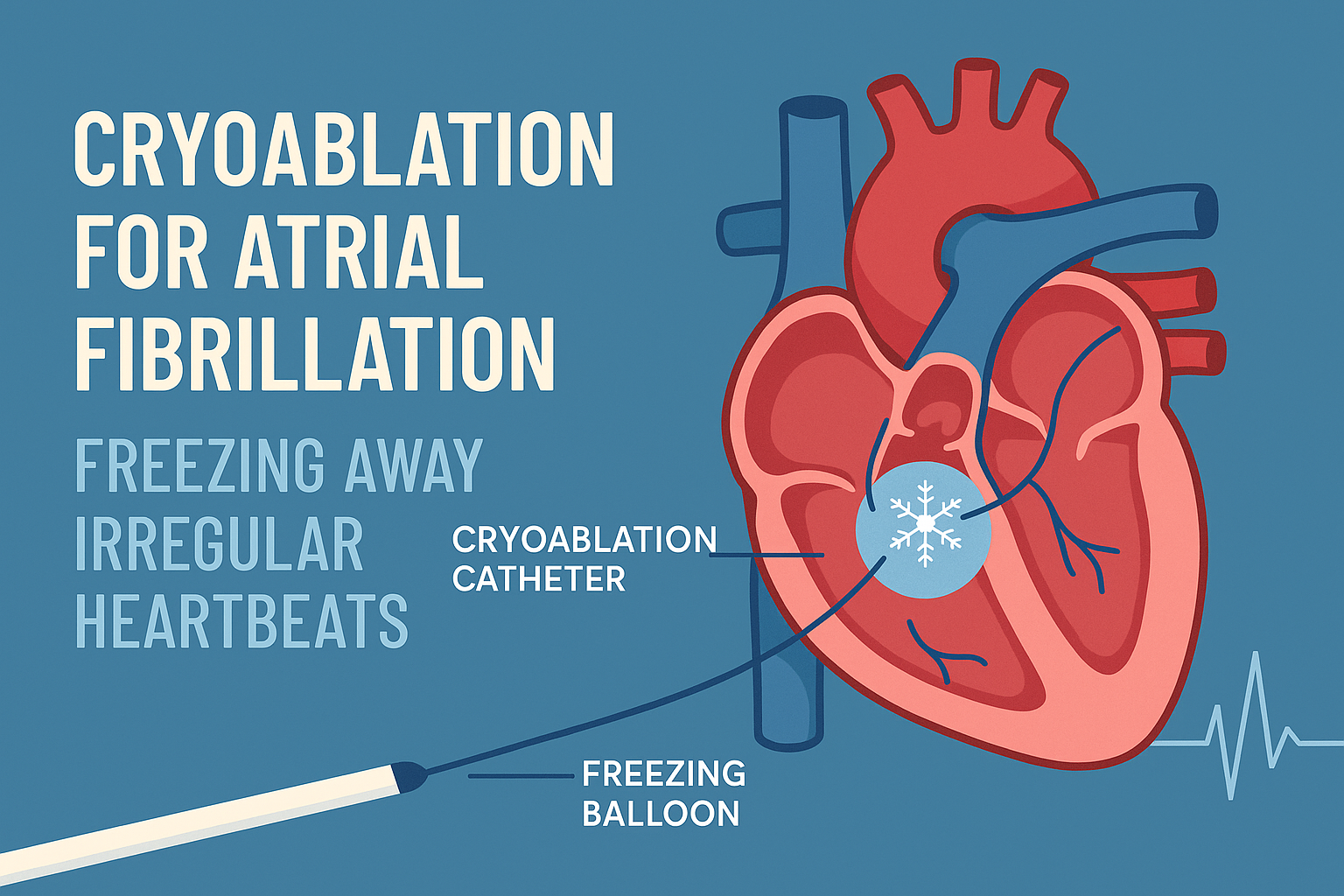
What is Cryoablation?
Cryoablation is a cold-based cardiac ablation technique. Instead of using heat (as in radiofrequency ablation), it freezes specific areas of heart tissue that trigger abnormal electrical signals.
The main targets are the pulmonary veins, where faulty impulses often originate.
By isolating these veins electrically, cryoablation restores normal rhythm.
How it Works
-
A balloon catheter is guided into the heart via a vein in the groin.
-
The balloon is inflated at the mouth of a pulmonary vein.
-
Extremely cold nitrous oxide is released, lowering tissue temperature to -50°C or lower.
-
The frozen tissue becomes scar tissue, permanently blocking faulty signals.
Cryoablation vs. Radiofrequency Ablation
| Aspect | Cryoablation (Freezing) | Radiofrequency Ablation (Heating) |
|---|---|---|
| Energy Source | Cold (nitrous oxide) | Heat (radio waves) |
| Lesion Creation | Single continuous freeze | Multiple point-by-point burns |
| Procedure Time | Shorter | Longer |
| Pain During Procedure | Usually less | Sometimes more |
| Pulmonary Vein Stenosis Risk | Lower | Slightly higher |
Who is a Good Candidate?
Best suited for:
-
Paroxysmal AF (episodes that start and stop spontaneously)
-
Patients symptomatic despite medications
-
Those seeking a minimally invasive, short-duration procedure
Not ideal for:
-
Permanent AF with large atrial scars
-
Patients unable to take blood thinners
Step-by-Step Procedure
-
Preparation – ECG, echocardiogram, CT scan, and lab work
-
Anesthesia – Usually general anesthesia
-
Access – Catheters inserted via the femoral vein
-
Transseptal Puncture – Small opening made between right and left atria
-
Balloon Placement – Positioned at each pulmonary vein opening
-
Freeze Cycle – Freezes tissue for 180–240 seconds per vein
-
Verification – Checks for complete electrical isolation
-
Recovery – Catheters removed, patient monitored overnight
Benefits of Cryoablation
-
Minimally invasive, no open surgery
-
Often shorter procedure time
-
Quick recovery — many patients back to routine within a week
-
Good long-term success for the right patients
-
Lower chance of pulmonary vein narrowing compared to heat-based methods
Risks and Considerations
-
Bleeding or bruising at catheter site
-
Phrenic nerve injury (rare, usually temporary)
-
Stroke (rare with proper anticoagulation)
-
Recurrence of AF (possible, may require repeat procedure)
Case Study: A 64-Year-Old’s Road to Recovery
Mr. R, a 64-year-old male, came to our hospital with recurrent palpitations despite being on rate- and rhythm-control medications.
He had:
-
Hypertension
-
Obesity
-
Mild obstructive sleep apnea (confirmed via sleep study)
Initial advice was weight reduction and risk factor control before intervention. But Mr. R planned to travel abroad soon and requested an early procedure.
We discussed:
-
Radiofrequency ablation
-
Cryoablation
After reviewing pros and cons, he chose Cryoablation.
Procedure: Under general anesthesia, we isolated all four pulmonary veins using the cryoballoon technique.
Outcome: Restored to sinus rhythm, stable post-procedure, and discharged the next day.
Follow-up: Remains symptom-free at 3 months, continues lifelong anticoagulation.
Life After Cryoablation
-
Anticoagulants continue lifelong if stroke risk is high
-
Lifestyle changes — weight loss, sleep apnea treatment, BP control — are essential
-
Regular follow-ups to monitor for recurrence
FAQs on Cryoablation for Atrial Fibrillation
Q1: Is cryoablation painful?
No — the procedure is usually done under general anesthesia or conscious sedation. You won’t feel the freezing.
Q2: How long does the procedure take?
Typically 2–3 hours, depending on anatomy and complexity.
Q3: What is the success rate?
For paroxysmal AF, success rates can be 70–80% after a single procedure, higher with repeat procedures.
Q4: Will I still need medication after cryoablation?
You may still need blood thinners to prevent stroke, depending on your risk score. Some may need anti-arrhythmic drugs temporarily.
Q5: Can AF come back after cryoablation?
Yes, there is a small chance of recurrence, especially in the first 3 months (blanking period) or years later.
Q6: How soon can I return to normal activities?
Most people return to normal life within a week, avoiding heavy lifting for a short time.
Q7: Is cryoablation safer than radiofrequency ablation?
Both are safe when done by experienced operators. Cryoablation has slightly lower risk of certain complications like pulmonary vein narrowing.
Q8: Does cryoablation cure AF permanently?
It can provide long-term relief for many, but no procedure guarantees 100% permanent cure.