By Dr. M.S. Chandramouli | MD, DM, IDCCM, PDF(EP), ECDS | Consultant Electrophysiologist & Heart Failure Specialist | Yashoda Hospitals – Secunderabad | ☎ 906 342 0686
Atrial fibrillation (AF) is one of the most common heart rhythm disorders affecting millions worldwide. Over the last decade, catheter ablation has become a cornerstone therapy for patients who continue to have symptoms despite medication. But the field is evolving rapidly—and one of the most exciting advancements today is High-Power Short-Duration (HPSD) ablation paired with high-resolution electroanatomical mapping.
This blog dives deep into how modern EP labs combine cutting-edge 3D mapping, pre-ablation voltage analysis, and strategic lesion creation using HPSD, and how post-ablation maps confirm success and durability of pulmonary vein isolation (PVI).
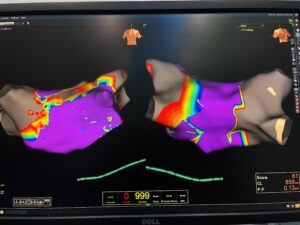
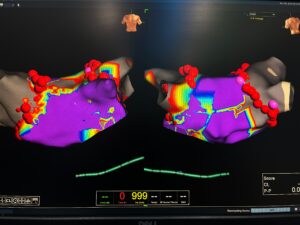
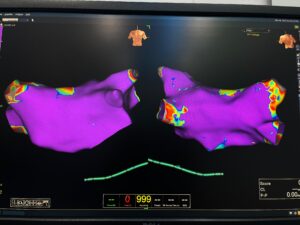
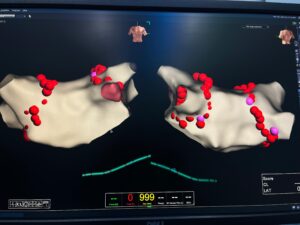
The process illustrated in the images—featuring detailed voltage maps before and after ablation—demonstrates exactly how far AF ablation has come.
Understanding AF Ablation: From “Burning Lines” to Precision Lesion Engineering
Traditional AF ablation typically uses 20–35 watts for longer durations (20–40 seconds). While effective, it has limitations:
-
Slower lesion creation
-
Higher chance of incomplete lesions
-
Greater risk of collateral tissue damage
-
Longer procedure time
Modern electrophysiology has shifted toward a precision-based approach using HPSD:
⭐ **High-Power (45–70 W)
⭐ Short-Duration (5–10 seconds)**
Instead of slowly heating deeper tissue, HPSD rapidly creates wide, shallow, contiguous lesions. This minimizes unwanted thermal spread but ensures effective pulmonary vein isolation.
When paired with real-time 3D mapping, the result is a safer, more durable, and more predictable ablation outcome.
Why Mapping Matters: Voltage, Activation & Lesion Integrity
Electroanatomical mapping systems—like CARTO, NavX, or Rhythmia—allow electrophysiologists to build a 3D model of the left atrium using millions of data points. The images you shared are classic examples of:
-
Voltage maps (purple areas = healthy tissue; red/yellow = scar, low voltage, fibrosis)
-
Lesion marker maps (red spheres indicating ablation points)
-
Pre- vs Post-ablation comparison
Pre-ablation Mapping helps identify:
✔ Pulmonary vein anatomy
✔ Areas of low voltage or fibrosis
✔ Regions where AF circuits may anchor
✔ Gaps from previous ablations (if redo case)
✔ Safe zones vs high-risk zones
Post-ablation Mapping confirms:
✔ Durable pulmonary vein isolation
✔ Absence of conduction gaps
✔ Lesion continuity
✔ Electrical silence in targeted areas
✔ Successful substrate modification
Step-By-Step Walkthrough of an HPSD AF Ablation Procedure
Below is a detailed narrative of how a modern AF ablation is performed using HPSD and mapping—perfect for patient education, medical blogs, or doctor websites.
1. Patient Preparation & 3D Left Atrial Reconstruction
After vascular access and transseptal puncture, a mapping catheter is advanced into the left atrium.
The system acquires thousands of data points in seconds, creating:
-
Chamber geometry
-
Voltage map
-
Activation patterns
In the images, the purple areas represent normal, healthy atrial muscle, while the rainbow edges (yellow–red) indicate low-voltage zones.
This helps the physician plan ablation strategy tailored to the patient’s anatomy.
2. Identifying the Arrhythmogenic Substrate
Before ablation, the voltage map shows:
-
Normal voltage zones: stable conduction
-
Low-voltage areas: fibrosis, diseased myocardium
-
Potential drivers of AF
Such maps help personalize the ablation plan.
For example:
-
In persistent AF, there may be extensive fibrosis.
-
Some patients have asymmetrical pulmonary vein anatomy.
-
Others may require additional lines beyond standard PVI.
3. Pulmonary Vein Isolation (PVI) with HPSD
This is the core step of AF ablation.
Why HPSD Works Better:
-
Creates shallow, wide lesions—ideal for PVI
-
Minimizes risk of injury to deeper structures like the esophagus
-
Produces uniform lesion sets
-
Reduces procedure time significantly
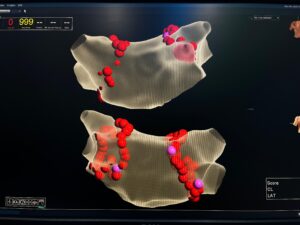
During ablation, each lesion is marked as a red sphere on the map (seen in the images).
The goal is to form a continuous, gap-free ring around each pulmonary vein pair.
The Benefits of HPSD PVI:
✔ Faster
✔ Safer
✔ More controlled
✔ More consistent lesion quality
✔ Lower chance of reconnection
4. Confirming Electrical Isolation – Post-Ablation Mapping
Once PVI is completed, the EP physician will:
-
Re-map the left atrium
-
Check if pulmonary veins are electrically isolated
-
Verify that no conduction gaps exist
-
Confirm absence of breakthrough signals
In the post-ablation maps you provided:
-
Areas that previously showed conduction now appear electrically silent
-
Lesion spheres form complete rings
-
Voltage in the targeted zones drops dramatically
This ensures the ablation is durable and effective, reducing the chance of AF recurrence.
5. Substrate Modification (if required)
In persistent or long-standing AF, substrate modification may be added:
-
Posterior wall isolation
-
Low-voltage area homogenization
-
Linear ablation (roof line, mitral isthmus)
-
Ablation of focal triggers
The images show additional lesion sets along areas of conduction abnormalities—precisely targeted using mapping data.
6. Final Remapping – The “End-Product”
After all lesion sets are completed:
-
A final left atrial map is created
-
Electrical activity is reassessed
-
All pulmonary veins should be isolated
-
Low-voltage areas are neutralized
-
No gap is left behind
This final map is crucial because the more complete the lesion set, the lower the recurrence rate.
The last images (beige 3D surfaces with red lesion points) show the final lesion set—clean, contiguous, and anatomically precise.
HPSD AF Ablation: Why It Matters for Patients
1. Higher Success Rates
Because lesions are more precise, durable, and consistent.
2. Faster Procedure
Less time inside the left atrium means:
-
Lower complication risk
-
Less anesthesia
-
Faster recovery
3. Safer for Surrounding Structures
Shorter energy delivery limits collateral damage.
4. Better for Thick or Fibrotic Tissue
High power helps overcome difficult-to-ablate regions.
5. More Durable Pulmonary Vein Isolation
The #1 factor affecting AF recurrence.
What the Mapping Images Reveal (Patient-Friendly Explanation)
If this blog is being used for patient education, here’s a simple explanation:
-
The purple areas show healthy heart tissue.
-
The yellow/red areas show weak or damaged tissue.
-
The red dots show where the doctor applied energy to correct AF.
-
After the procedure, the map becomes more uniform, meaning AF triggers are controlled.
Why Pre- and Post-Mapping Should Be Standard of Care
Mapping before and after ablation is no longer optional—it is essential.
Pre-Ablation Mapping
✔ Identifies fibrosis
✔ Localizes triggers
✔ Personalizes strategy
Post-Ablation Mapping
✔ Confirms electrical success
✔ Ensures no gaps
✔ Reduces recurrence
✔ Provides measurable outcomes
When combined with HPSD, the results are significantly enhanced.
FAQs on AF Ablation Using HPSD and Mapping
1. What is HPSD ablation?
HPSD stands for High-Power Short-Duration ablation. It uses higher energy (45–70 W) for very short durations (5–10 seconds) to create fast, shallow, precise lesions that isolate AF triggers.
2. Is HPSD safe?
Yes. In fact, it is often safer than traditional methods because:
-
Heat does not penetrate deep tissues
-
Esophageal injury risk is lower
-
Lesions are more consistent
-
Total procedure time decreases
3. Why is mapping needed for AF ablation?
Mapping shows:
-
Electrical signals
-
Tissue health
-
Fibrosis
-
Pulmonary vein conduction
It ensures the ablation is customized and effective.
4. What do the colors on the map mean?
-
Purple – healthy tissue
-
Yellow/Red – scar or low voltage
-
Red spheres – ablation lesions
5. How long does an HPSD AF ablation take?
Typically 1–2 hours, depending on whether additional lines or substrate modification is needed.
6. Can AF return after ablation?
While no procedure is 100% guaranteed, HPSD + mapping significantly reduces recurrence rates by ensuring durable lesions.
7. What is pulmonary vein isolation (PVI)?
PVI is the process of electrically separating the pulmonary veins from the rest of the left atrium so they cannot trigger AF.
8. Will I feel better immediately after ablation?
Many patients notice improvement within days, but healing takes 8–12 weeks. During this time, occasional irregular beats are normal.
9. Who is a good candidate for HPSD ablation?
Patients with:
-
Symptomatic paroxysmal AF
-
Persistent AF
-
Intolerance to antiarrhythmic drugs
-
Recurrent AF after previous ablation
10. Is this a long-term cure for AF?
Ablation significantly improves long-term rhythm control and reduces dependence on medications. Many patients remain arrhythmia-free for years.
The combination of HPSD ablation with pre- and post-procedural electroanatomical mapping represents the highest standard in modern electrophysiology. It brings together:
-
Faster lesion creation
-
Safer techniques
-
More reliable isolation
-
Lower recurrence rates
-
Personalized therapy tailored to each patient’s atrial substrate
The images of pre- and post-ablation mapping highlight exactly how technology has transformed cardiac arrhythmia treatment—turning the left atrium into a fully measurable, understandable, and treatable structure.
With tools like HPSD and 3D mapping, AF ablation today is not just a procedure—it’s precision engineering of heart rhythm, designed for long-term success and improved quality of life.