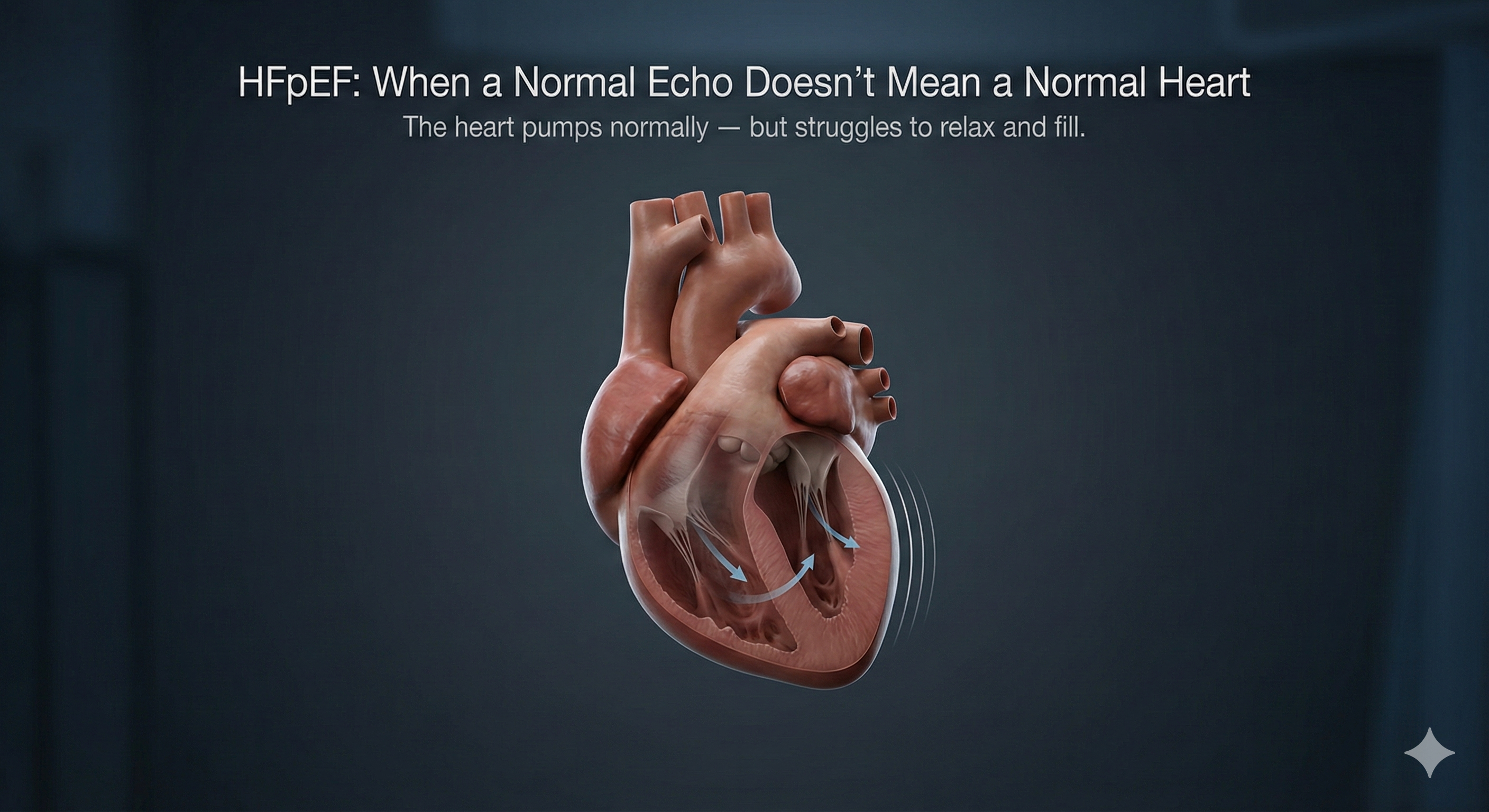
Heart failure is often misunderstood as a condition where the heart becomes weak and cannot pump blood effectively. While this is true for many patients, there is an important and increasingly common form of heart failure where the heart’s pumping function appears normal on tests. This condition is called Heart Failure with Preserved Ejection Fraction (HFpEF).
HFpEF is a challenging and often underdiagnosed condition. Patients may be told that their echocardiogram is “normal,” yet they continue to experience troubling symptoms such as breathlessness, fatigue, and exercise intolerance. Understanding HFpEF is crucial for timely diagnosis, appropriate treatment, and improved quality of life.
This blog explains HFpEF in detail—what it is, why it happens, how it is diagnosed, and how it is managed in modern cardiology practice.
What Is HFpEF?
HFpEF stands for Heart Failure with Preserved Ejection Fraction.
Ejection fraction (EF) is the percentage of blood the heart pumps out with each beat. In HFpEF, the EF is usually 50% or higher, which is considered normal.
The problem in HFpEF is not pumping, but filling.
In this condition:
-
The heart muscle becomes stiff or less compliant
-
The heart does not relax properly between beats
-
The chambers cannot fill adequately with blood
-
Pressure builds up in the heart and lungs
Despite normal pumping strength, the heart fails to meet the body’s demands, leading to heart failure symptoms.
Why HFpEF Is Often Missed
HFpEF is frequently overlooked because:
-
The echocardiogram shows a normal ejection fraction
-
Symptoms may be subtle or gradual
-
Breathlessness is often blamed on age, weight, or lung problems
-
Routine tests may appear “reassuring”
Many patients are told that their heart is fine, even though their daily activities are limited by fatigue or shortness of breath. This delay in recognition can result in worsening symptoms and repeated hospital visits.
Common Symptoms of HFpEF
Symptoms of HFpEF are similar to other forms of heart failure and may include:
-
Breathlessness during exertion or at rest
-
Easy fatigability
-
Reduced exercise capacity
-
Swelling of ankles or legs
-
Rapid weight gain due to fluid retention
-
Night-time breathlessness or disturbed sleep
Symptoms often worsen with physical activity or fluid overload and may fluctuate over time.
Who Is at Risk of Developing HFpEF?
HFpEF is more common in certain groups of patients, especially:
-
Older adults
-
Long-standing high blood pressure
-
Diabetes mellitus
-
Obesity and metabolic syndrome
-
Chronic kidney disease
-
Atrial fibrillation
-
Women, particularly post-menopausal
These conditions contribute to stiffening of the heart muscle and abnormal relaxation, which are central to HFpEF.
How HFpEF Develops
HFpEF usually develops gradually. Chronic conditions such as hypertension and diabetes cause structural and functional changes in the heart over time. These include:
-
Thickening of the heart muscle
-
Increased fibrosis (scarring)
-
Reduced elasticity of the heart chambers
-
Elevated filling pressures
As a result, even normal daily activities can cause breathlessness because the heart cannot accommodate increased blood flow during exertion.
Diagnosing HFpEF: Beyond the Ejection Fraction
Diagnosing HFpEF requires careful clinical evaluation. A normal ejection fraction alone does not rule out heart failure.
Diagnosis typically involves:
-
Detailed clinical history and symptom assessment
-
Echocardiography focusing on diastolic function
-
Measurement of heart chamber sizes and filling pressures
-
Blood tests such as natriuretic peptides
-
Evaluation of associated conditions like hypertension and atrial fibrillation
In some cases, advanced imaging or stress testing may be required to confirm the diagnosis.
Why HFpEF Is a Challenging Condition
HFpEF is complex because:
-
It has multiple contributing factors
-
Patients often have several co-existing medical conditions
-
Symptoms vary widely between individuals
-
No single treatment works for all patients
Management therefore requires a personalized, long-term approach rather than a one-size-fits-all solution.
Treatment Goals in HFpEF
The main goals of HFpEF management are:
-
Relief of symptoms
-
Prevention of fluid overload
-
Reduction in hospital admissions
-
Improvement in exercise tolerance
-
Management of underlying risk factors
Unlike heart failure with reduced ejection fraction, treatment in HFpEF focuses more on controlling contributing conditions and optimizing heart function.
Medical Management of HFpEF
Treatment strategies may include:
-
Careful control of blood pressure
-
Diuretics to manage fluid retention
-
Heart rate control, especially in atrial fibrillation
-
Newer heart failure medications shown to improve outcomes
-
Optimal management of diabetes and kidney disease
Regular follow-up is essential to adjust therapy based on symptoms and response to treatment.
Lifestyle Modifications That Matter
Lifestyle changes play a crucial role in HFpEF management. Patients are often advised to:
-
Follow a low-salt diet
-
Maintain a healthy body weight
-
Engage in supervised, regular physical activity
-
Monitor daily weight for fluid retention
-
Avoid excess alcohol and smoking
Even small improvements in lifestyle can significantly reduce symptoms and improve daily functioning.
Role of Specialized Heart Failure Care
Because HFpEF is complex, care under a specialist experienced in heart failure and rhythm disorders is essential. Expert evaluation ensures accurate diagnosis, appropriate medication selection, and close monitoring over time.
At centers like Yashoda Hospitals, patients benefit from integrated heart failure care guided by specialists such as Dr. M.S. Chandramouli, who focuses on both heart rhythm disorders and advanced heart failure management.
Living with HFpEF
HFpEF is a chronic condition, but with the right approach, many patients can lead active and fulfilling lives. Early diagnosis, adherence to treatment, and regular follow-up are key to long-term stability.
Patients should seek medical attention promptly if symptoms worsen, as early intervention can prevent hospitalizations and complications.
Frequently Asked Questions (FAQs)
1. Can I have heart failure if my echocardiogram is normal?
Yes. In HFpEF, the ejection fraction is normal, but the heart’s ability to relax and fill is impaired, leading to heart failure symptoms.
2. Is HFpEF serious?
HFpEF is a serious condition that can significantly affect quality of life and lead to repeated hospitalizations if not properly managed.
3. Is HFpEF the same as diastolic heart failure?
Yes. HFpEF is commonly referred to as diastolic heart failure because the main problem occurs during the heart’s relaxation phase.
4. Who commonly develops HFpEF?
HFpEF is more common in older adults, patients with long-standing hypertension, diabetes, obesity, kidney disease, and atrial fibrillation.
5. Can HFpEF be cured?
HFpEF cannot be completely cured, but symptoms can be effectively controlled with proper medical care, lifestyle changes, and regular monitoring.
6. What tests are used to diagnose HFpEF?
Diagnosis involves clinical evaluation, echocardiography focused on diastolic function, blood tests, and assessment of associated conditions.
7. Does HFpEF require lifelong treatment?
Yes. HFpEF is a chronic condition and usually requires long-term treatment and follow-up to maintain symptom control and prevent complications.
Dr. M.S. Chandramouli
MD, DM, IDCCM, PDF (EP), ECDS
Consultant Electrophysiologist & Heart Failure Specialist
Yashoda Hospitals – Secunderabad
Dr. M.S. Chandramouli is a highly experienced cardiac electrophysiologist and heart failure specialist with over 7 years of focused expertise in managing complex heart rhythm disorders and advanced heart failure conditions. He is known for combining precision-driven technology with compassionate, patient-centric care.
Clinical Expertise & Experience
-
1200+ Radiofrequency Ablation (RFA) and 3D Mapping Procedures
-
800+ Cardiac Device Implantations, including pacemakers, ICDs, and CRT devices
-
Specialized in atrial fibrillation, complex arrhythmias, and heart failure (including HFpEF)
-
Expertise in advanced electrophysiology studies and device-based therapies
Areas of Special Interest
-
Cardiac arrhythmias and rhythm disorders
-
Heart failure management, including HFpEF and advanced heart failure
-
Pacemaker, ICD, and CRT implantation and follow-up
-
Comprehensive rhythm and heart failure care under one roof