Atrial arrhythmias in patients with prior coronary artery bypass grafting (CABG) can be complex, challenging, and often recurrent. Scar-related circuits, atrial remodeling, and structural heart disease make diagnosis and management significantly more demanding. This case highlights an atypical left atrial (LA) flutter successfully diagnosed and treated using advanced electrophysiological study (EPS), high-density (HD) mapping, and radiofrequency ablation (RFA).
Clinical Background
A 62-year-old male with a history of coronary artery disease (CAD) underwent CABG five years earlier with three saphenous vein grafts (SVG). He presented with:
-
Recurrent episodes of supraventricular tachycardia (SVT)
-
Heart rate reaching 200 bpm
-
Symptoms of palpitations and breathlessness
-
No episodes of syncope
Echocardiography revealed:
-
Moderate left ventricular (LV) dysfunction
-
Ejection fraction (EF) of 40%
-
Mild mitral regurgitation (MR)
-
Mild tricuspid regurgitation (TR)
Given recurrent symptomatic tachycardia, the plan was to proceed with Electrophysiology Study (EPS) and 3D-guided Radiofrequency Ablation (RFA).
Baseline ECG and Intracardiac Electrograms
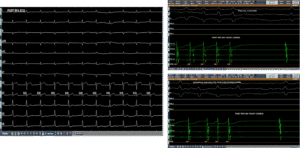
As seen in the baseline ECG and intracardiac electrograms (Page 3 of the case file), the patient demonstrated narrow complex tachycardia with organized atrial activity. Intracardiac recordings showed consistent atrial activation patterns suggestive of a re-entrant arrhythmia rather than focal atrial tachycardia.
This distinction is critical because re-entrant tachycardias require identification of a circuit and interruption of the critical isthmus for definitive treatment.
Induction and Entrainment: Confirming the Diagnosis
During the electrophysiology study (Page 4), tachycardia was induced using programmed stimulation.
Ventricular entrainment pacing demonstrated a VAAV response, confirming an atrial tachycardia/atrial flutter mechanism. The tachycardia cycle length (TCL) was approximately 310 ms.
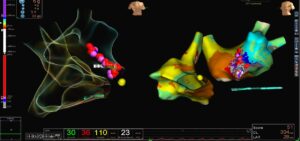
Since atrial flutter typically represents a macro re-entrant circuit, mapping of both right atrium (RA) and left atrium (LA) was planned using a high-density grid catheter to create a Local Activation Time (LAT) map.
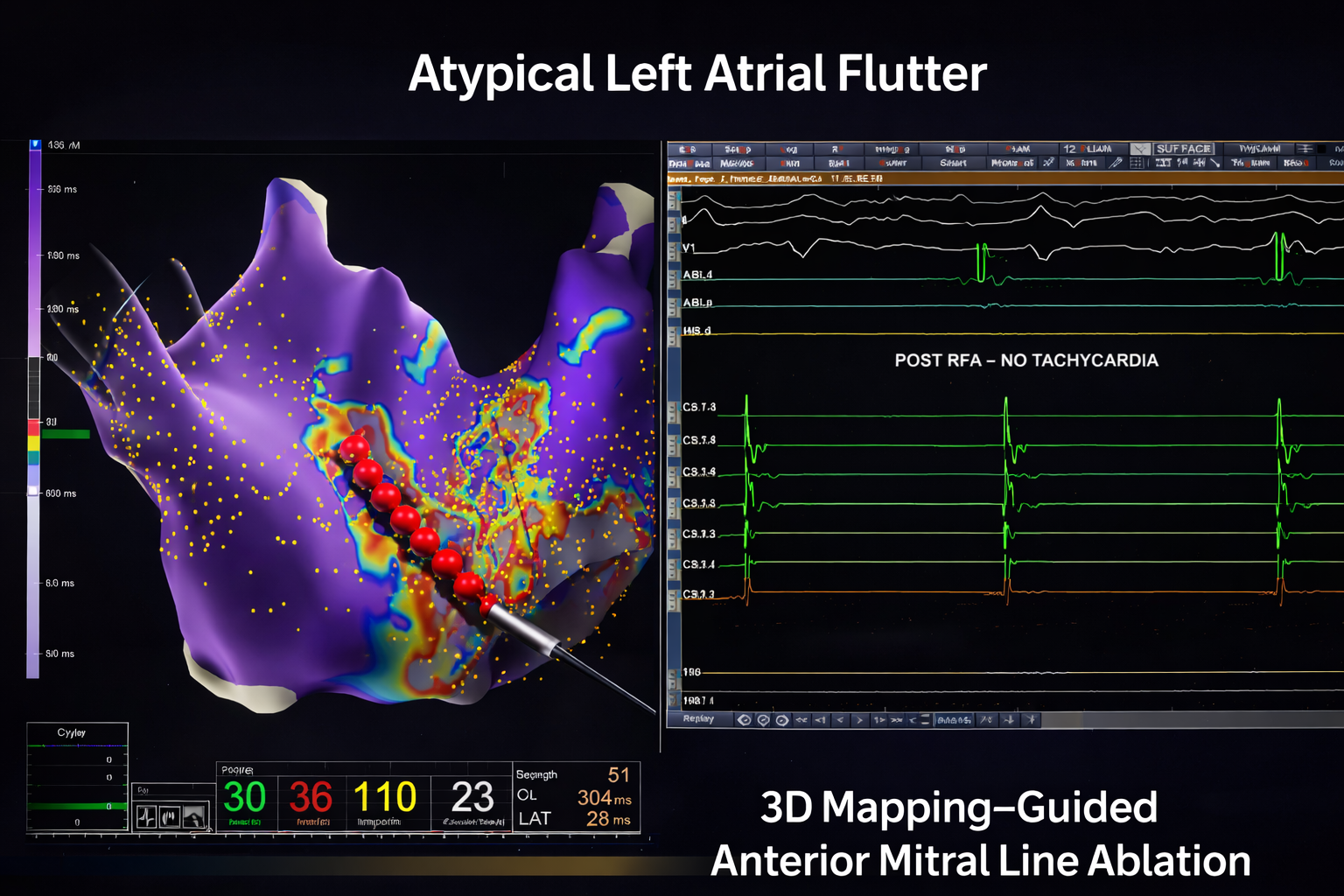
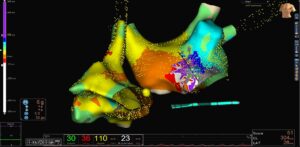
3D LAT Activation Mapping: Identifying the Circuit
LAT activation mapping demonstrated a macro re-entrant circuit in the left atrium.
Key observations:
-
Activation spanned nearly the entire tachycardia cycle length
-
High-density grid signals covered approximately 190 ms
![]()
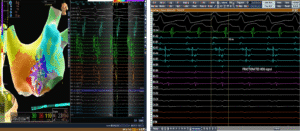
-
The mapping confirmed a scar-related re-entry pattern
-
Propagation mapping showed wavefront circulation consistent with atypical LA flutter
In post-CABG patients, surgical scarring and atrial remodeling often create slow-conduction channels. These channels act as substrates for re-entry.
The propagation map clearly visualized wavefront movement around a scar region, confirming the arrhythmia was left atrial in origin rather than typical right atrial cavotricuspid isthmus flutter.
High-density mapping revealed:
-
Fractionated electrograms
-
Late potentials
-
Areas of low voltage consistent with atrial scar
These findings are characteristic of atypical LA flutter circuits. Fractionated signals indicate zones of slow conduction — the critical substrate maintaining re-entry.
Interestingly, the HD grid catheter mechanically “bumped” the tachycardia, leading to termination.
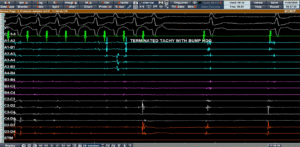
Despite attempts, tachycardia could not be reinduced easily, further supporting a fragile re-entrant substrate dependent on a specific conduction channel.
Ablation Strategy: Correlation with ILAM and Voltage Map
The ablation strategy involved correlating:
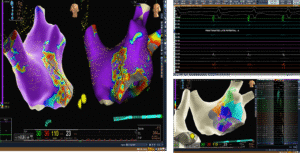
-
Isochronal Late Activation Mapping (ILAM)
-
Voltage mapping of the left atrium
The critical isthmus was identified along the anterior mitral region.
An anterior mitral line was drawn using an irrigated ablation catheter with:
-
Power: 35 W
-
Temperature: 43°C
As shown on, the linear lesion connected anatomical landmarks to interrupt the re-entry circuit permanently.
Creating a complete conduction block across this line is essential to prevent recurrence.
Post-Ablation Assessment
Post-RFA ECG demonstrated sinus rhythm.
Aggressive tachycardia induction protocols were performed, including:
-
Burst pacing
-
Programmed stimulation
No tachycardia could be re-induced.
This confirmed successful ablation and electrical stability.
Key Learning Points
1. Atypical LA Flutter is Common in Post-Surgical Hearts
Prior CABG and structural heart disease create atrial scarring, forming substrates for macro re-entry.
2. Entrainment is Essential for Mechanism Confirmation
VAAV response during ventricular pacing confirmed atrial origin.
3. 3D Mapping is Crucial
Conventional mapping would likely miss complex left atrial circuits. High-density mapping enables:
-
Precise localization
-
Identification of slow conduction channels
-
Targeted ablation
4. ILAM and Voltage Correlation Improves Accuracy
Combining activation and voltage data identifies the true critical isthmus.
5. Linear Ablation Remains the Cornerstone
Anterior mitral line ablation effectively interrupted the macro re-entry circuit.
Dr. M.S. Chandramouli
MD, DM, IDCCM, PDF (EP), ECDS
Consultant Electrophysiologist & Heart Failure Specialist
Hospital: Yashoda Hospitals – Secunderabad
Address: Alexander Rd, Kummari Guda, Shivaji Nagar, Secunderabad, Telangana 500003
Phone: 906 342 0686
Hours: Open 24 hours