Catheter ablation is a revolutionary, minimally invasive procedure that has transformed the way atrial fibrillation (AF) is treated—especially when medications fail to control the condition. Yet, despite its increasing adoption and promising results, many patients remain apprehensive or confused about the procedure.
In this blog, we’ll address the most common concerns patients express about catheter ablation, demystify the process, highlight its benefits and risks, and provide the facts you need to make an informed decision. Whether you’re considering catheter ablation for yourself or supporting a loved one, this article will help guide you through the journey.
What Is Catheter Ablation?
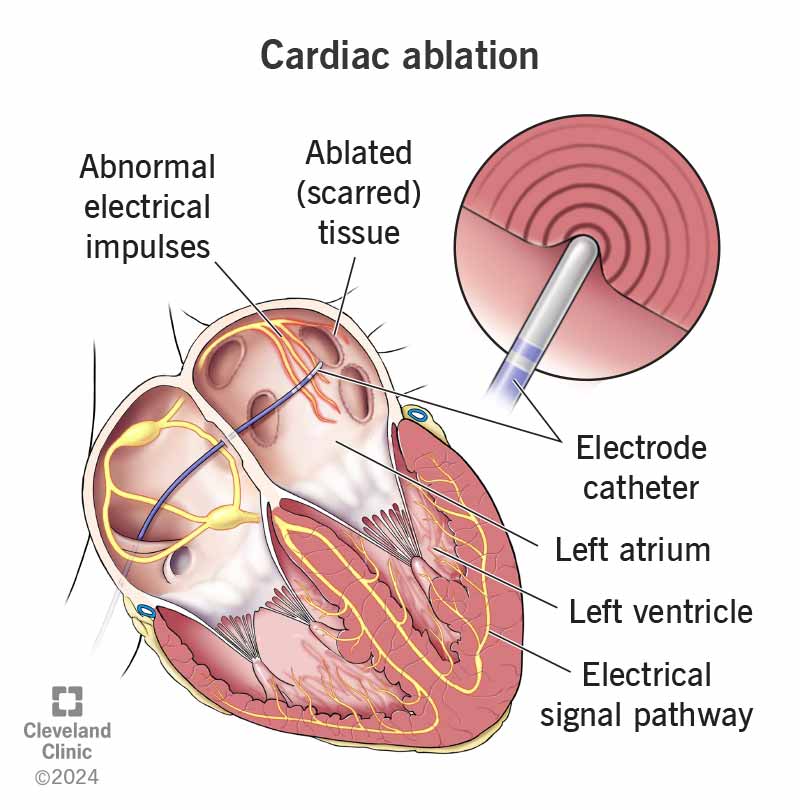
Catheter ablation is a procedure performed by electrophysiologists (heart rhythm specialists) to treat irregular heartbeats, particularly atrial fibrillation. It involves guiding thin, flexible tubes (catheters) into the heart through blood vessels, most commonly via the groin. Once inside, the doctor delivers targeted energy—either radiofrequency (heat) or cryotherapy (cold)—to destroy small areas of heart tissue that are triggering abnormal electrical signals.
The aim is to restore normal heart rhythm, reduce symptoms such as palpitations, breathlessness, and fatigue, and decrease the need for ongoing medication.
Who Is a Candidate for Catheter Ablation?
According to current guidelines and clinical experience, catheter ablation is typically recommended for:
-
Patients with symptomatic atrial fibrillation (paroxysmal or persistent)
-
Individuals who did not respond to or cannot tolerate at least one antiarrhythmic medication
-
Patients at risk of complications from long-term AF, such as stroke or heart failure
While it is not usually the first line of treatment, ablation is an excellent option when lifestyle changes and medications aren’t effective or sustainable.
Common Patient Concerns—And What You Should Know
Let’s walk through some of the most frequently asked questions and concerns raised by patients when considering catheter ablation:
1. “I don’t understand what the procedure involves.”
You’re not alone. Medical procedures can be intimidating, especially those involving the heart. But catheter ablation is less invasive than many people imagine.
Here’s how it works:
-
You are given either general anesthesia or conscious sedation.
-
A small incision is made, typically in the groin.
-
Catheters are inserted and guided to the heart using imaging technology.
-
The physician maps the electrical pathways and identifies areas causing AF.
-
Targeted energy is delivered to these spots, disrupting the erratic signals.
-
Catheters are removed, and the incision is closed—no stitches typically required.
Most procedures last between 2 to 4 hours. Hospital stays are short, often overnight, and patients can resume normal activities within a few days.
2. “How does ablation help my condition?”
Atrial fibrillation results from disorganized electrical activity in the upper chambers of the heart. Medications may control these signals temporarily but often fail to address the root cause. Catheter ablation targets and eliminates the faulty areas directly.
Clinical studies show that:
-
70% of patients with paroxysmal AF are symptom-free 12 months after radiofrequency ablation.
-
In the STOP-AF trial, 69.9% of patients treated with cryoballoon ablation remained free of AF at 1 year—compared to only 7.3% of patients treated with drugs alone.
-
More than 74% of patients are able to stop antiarrhythmic medications after successful ablation.
This procedure isn’t just about rhythm control—it significantly improves quality of life, stamina, and long-term heart health.
3. “I’m scared to have heart surgery.”
Fear is natural, especially when it involves the heart. But it’s important to understand that catheter ablation is not open-heart surgery. There are:
-
No large incisions
-
No cutting of the chest
-
Minimal pain
-
Faster recovery than surgical alternatives
It is done in an electrophysiology (EP) lab, not an operating room. The incisions are typically the size of a pencil tip and heal within days.
Patients can often go home the same day or the next morning. Complications are rare, and you’ll be closely monitored during and after the procedure.
4. “What if the procedure doesn’t work?”
No procedure offers a 100% guarantee—but catheter ablation has a strong track record.
Success depends on several factors:
-
Type of AF (paroxysmal AF responds better than persistent AF)
-
How long you’ve had AF
-
Overall heart health
Some patients may need a second ablation if AF recurs, but overall outcomes are excellent. Long-term freedom from AF after one or two procedures exceeds 80% in many studies, especially when done early in the disease course.
5. “What are the risks?”
Like all medical procedures, catheter ablation comes with risks, though serious complications are uncommon. Potential risks include:
-
Bleeding or bruising at the catheter site
-
Infection
-
Damage to nearby structures (e.g., phrenic nerve)
-
Pulmonary vein stenosis (narrowing)
-
Pericardial tamponade (fluid around the heart)
-
Stroke (rare)
-
Atrio-esophageal fistula (very rare but serious)
Your care team will review these risks with you and take precautions to minimize them. Most patients have a smooth recovery without complications.
6. “My symptoms come and go—I don’t think I need treatment.”
Atrial fibrillation can be deceptive. Even if you don’t feel palpitations or fatigue regularly, untreated AF can silently increase your risk of:
-
Stroke (AF increases stroke risk by 5x)
-
Heart failure
-
Cognitive decline
-
Reduced life expectancy
That’s why cardiologists recommend addressing AF early—even in the absence of persistent symptoms. Treating it now may prevent complications later.
Clinical Evidence: Why Catheter Ablation Is Becoming the Preferred Option
Multiple landmark trials have shown that catheter ablation:
-
Offers better rhythm control than drugs
-
Reduces hospitalizations
-
Lowers stroke risk
-
Improves heart function
-
Enhances patient-reported quality of life
It is especially effective when performed early, before structural damage to the heart occurs. With improved technologies (like contact-force sensing and cryoballoons), outcomes are more consistent than ever.
What to Expect After the Procedure
Recovery is generally quick:
-
Most patients return home within 24 hours
-
Resume light activity in 2–3 days
-
Full recovery within 1–2 weeks
-
Some patients may experience mild chest discomfort or fatigue temporarily
You may still be on blood thinners and rhythm medications for a few weeks or months post-procedure, depending on your doctor’s plan. Regular follow-ups and rhythm monitoring (like Holter or ECG) will help assess long-term success.
Lifestyle After Ablation: What Changes?
For many, catheter ablation feels like a new lease on life. You may find:
-
Increased energy and exercise tolerance
-
Better sleep
-
Reduced anxiety about AF episodes
-
Fewer emergency visits
However, sustaining results means embracing a heart-healthy lifestyle:
-
Eat a balanced diet
-
Manage high blood pressure and diabetes
-
Avoid smoking and excess alcohol
-
Exercise regularly
-
Maintain a healthy weight
Ablation addresses the electrical problem, but lifestyle changes address the triggers.
Conclusion: Don’t Let Fear Stop You From Living Fully
Catheter ablation isn’t just a procedure—it’s a step toward freedom from the burdens of atrial fibrillation. If medications aren’t working, or you’re tired of living in fear of the next episode, it’s worth discussing this option with your electrophysiologist.
Yes, there are concerns. Yes, it’s normal to have questions. But today’s catheter ablation is safer, more effective, and more accessible than ever. With success rates up to 80%, minimal downtime, and the potential to discontinue medications, it has become a life-changing option for many patients.
FAQs About Catheter Ablation
Q1: Is catheter ablation painful?
Most patients are under sedation or general anesthesia and do not feel pain during the procedure. Post-procedure soreness in the groin area is common but mild.
Q2: Will I still need medications after ablation?
Some patients may still need blood thinners or rhythm medications initially, but many can discontinue them after successful ablation and follow-up.
Q3: Can AF come back after ablation?
Yes, recurrence can happen. However, the chances are significantly reduced, especially with early intervention. A second ablation may be needed in some cases.
Q4: Is catheter ablation safe for older adults?
Yes, it can be performed safely in patients over 65 or even 75, provided they are in good general health. Age alone is not a disqualifier.
Q5: How soon can I return to work or exercise?
Most patients resume work and light activities within a week. Full exercise routines can typically restart in 2–3 weeks based on doctor’s advice.