By Dr. M S ChandraMouli
Introduction
Tricuspid valve (TV) disease, though less common than left-sided valvular pathologies, can lead to significant morbidity, particularly when associated with congenital heart defects such as atrial septal defects (ASD). Surgical intervention, including bioprosthetic tricuspid valve replacement, is often required in advanced cases. However, postoperative complications such as complete heart block necessitate prompt management, often with permanent pacemaker (PPM) implantation.
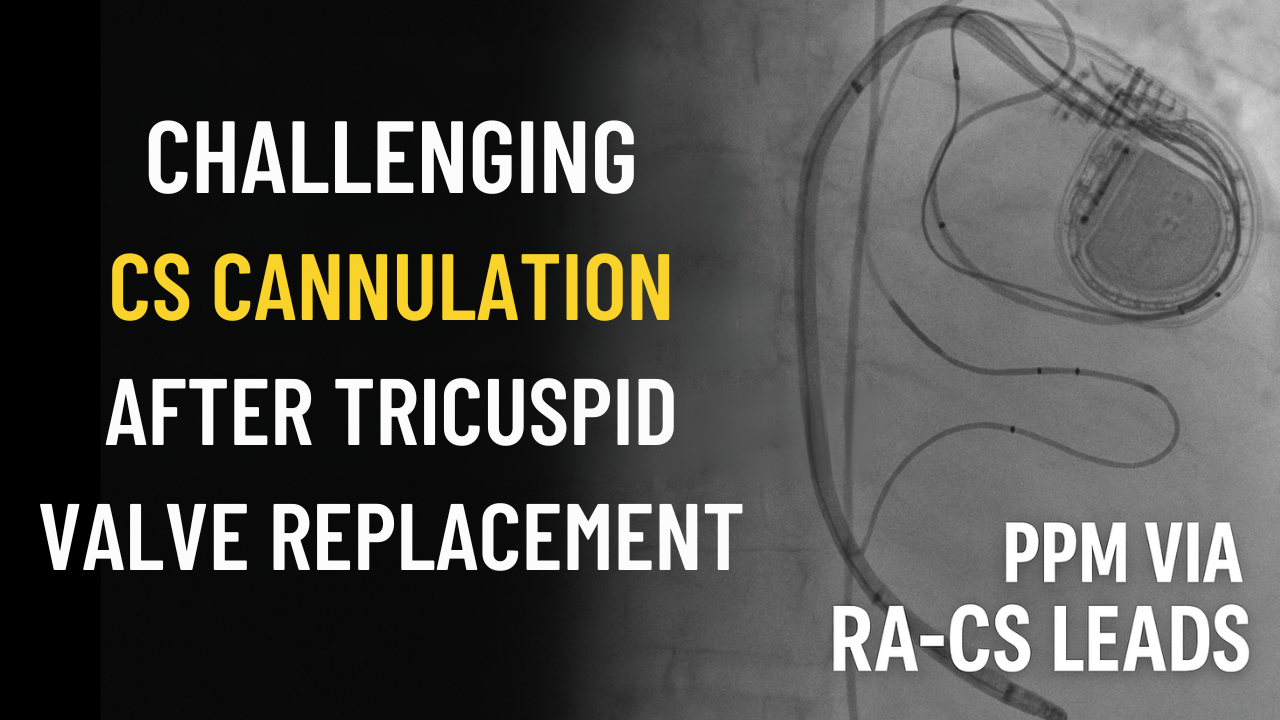
One challenging aspect of PPM implantation post-tricuspid valve replacement is the technical difficulty of coronary sinus (CS) lead cannulation, primarily due to anatomic changes and obstacles such as the presence of a Thebesian valve at the CS ostium. This blog explores a rare and instructive case of a female patient with ASD and organic tricuspid valve disease, who underwent bioprosthetic tricuspid valve replacement and subsequently developed complete heart block requiring PPM implantation via RA and CS leads. We’ll discuss the technical challenges faced, the solutions applied, and practical tips for electrophysiologists encountering similar cases.
Case Overview
The patient was a middle-aged female with a longstanding atrial septal defect and organic tricuspid valve disease. She underwent successful bioprosthetic tricuspid valve replacement surgery. Unfortunately, on postoperative day 7, she developed complete heart block, a known but serious complication following tricuspid valve surgery.
Given the conduction disturbance, a permanent pacemaker was indicated. Traditional right ventricular (RV) lead placement was complicated by the new bioprosthetic valve. Thus, an alternative strategy involving lead placement in the right atrium (RA) and coronary sinus (CS) was pursued.
The Challenges of Post-Tricuspid Valve Replacement Pacing
Why Is Pacing Difficult After Tricuspid Valve Replacement?
-
Mechanical Obstruction: The prosthetic valve physically impedes passage of pacing leads across the tricuspid annulus into the RV.
-
Risk of Valve Damage: Crossing the valve with leads may increase the risk of damaging the bioprosthesis or causing valve dysfunction.
-
Altered Anatomy: Surgical manipulation may alter RA and CS anatomy, making lead navigation more complex.
-
Conduction System Damage: Tricuspid valve surgery often involves areas near the atrioventricular (AV) node, increasing the risk of conduction block.
These factors necessitate innovative pacing approaches, such as placing a CS lead for left ventricular or posterolateral vein pacing, combined with RA lead placement to ensure atrial sensing.
Coronary Sinus Cannulation: The Thebesian Valve Challenge
The coronary sinus, a large venous structure collecting blood from the myocardium, opens into the right atrium through the CS ostium, which is guarded by a thin but sometimes fenestrated structure called the Thebesian valve. This valve can present a significant obstacle for catheter and lead cannulation.
The Thebesian Valve
-
It is a semicircular fold of tissue at the CS ostium.
-
Present in ~70-80% of individuals but varies widely in morphology.
-
Can partially or completely cover the CS ostium, making lead entry difficult or impossible without special maneuvers.
In this patient, the presence of a prominent Thebesian valve was a major hurdle for cannulating the CS ostium and advancing the pacing lead.
Technical Strategy for Successful Lead Placement
The key technical insights and tools used in this case included:
1. Use of AL2 Catheter
-
The Amplatz Left 2 (AL2) catheter was chosen for its shape and support.
-
Its design allows better alignment and support against the atrial wall near the CS ostium.
-
This catheter provides the necessary backup force to engage the CS ostium despite the valve obstruction.
2. Terumo Wire
-
A hydrophilic Terumo guidewire was used for its flexibility and trackability.
-
The wire easily negotiated the Thebesian valve fenestrations and passed into the CS.
-
The smooth surface of the wire reduces trauma and helps negotiate tortuous anatomy.
3. Targeting the Posterolateral Vein
-
The posterolateral vein was selected for lead placement due to favorable anatomy and pacing parameters.
-
After successful CS cannulation, advancing the lead into this branch ensured optimal pacing thresholds and stability.
4. Careful Manipulation
-
Gentle, controlled catheter and wire manipulation minimized the risk of trauma or dislodgment.
-
Fluoroscopic guidance was critical to ensure the catheter and lead remained in the proper plane.
Outcomes and Learnings
The permanent pacemaker implantation was successful with RA lead and CS lead placed in the posterolateral vein. The patient’s complete heart block was effectively managed without compromising the tricuspid valve prosthesis or causing additional complications.
This case highlights several important considerations for electrophysiologists:
-
Pre-procedural planning: Understanding patient-specific anatomy via imaging can guide catheter and lead selection.
-
Specialized tools: AL2 catheters and hydrophilic wires are invaluable in difficult cannulations.
-
Avoiding valve damage: Alternative pacing sites such as CS branches can bypass the tricuspid valve prosthesis.
-
Patience and precision: Difficult anatomy requires slow, meticulous technique.
Practical Tips for Electrophysiologists
-
Anticipate challenges in post-tricuspid valve surgery patients. Expect the presence of Thebesian valves and altered RA anatomy.
-
Use appropriate catheters. AL2 or similar support catheters often provide the required backup force for CS ostium engagement.
-
Select guidewires carefully. Hydrophilic, atraumatic wires like the Terumo improve maneuverability and reduce endothelial trauma.
-
Consider posterolateral or other CS tributaries as pacing sites to avoid crossing the prosthetic valve.
-
Fluoroscopy is your friend. Multiple views (LAO, RAO) help navigate complex anatomy.
-
Coordinate with the surgical team. Knowledge of the exact prosthetic valve type and surgical modifications can aid procedural planning.
-
Be prepared for longer procedure times. Challenging cannulations require patience and endurance.
Summary
Permanent pacemaker implantation after tricuspid valve replacement presents unique challenges, particularly with coronary sinus cannulation. The presence of an obstructive Thebesian valve can complicate CS access, but with appropriate tools such as the AL2 catheter and Terumo hydrophilic wire, successful lead placement is achievable.
Placing leads in the posterolateral vein via the CS allows pacing without crossing the prosthetic tricuspid valve, preserving valve integrity and ensuring effective conduction support in patients with postoperative heart block.
This case underlines the importance of a thorough understanding of cardiac anatomy, specialized equipment, and careful technique in managing complex electrophysiological challenges after valve surgery.
Frequently Asked Questions (FAQs)
Q1: Why is permanent pacemaker implantation difficult after tricuspid valve replacement?
A: The prosthetic valve physically blocks the passage of leads into the right ventricle, and crossing it risks valve damage. Hence, alternative lead placement sites like the coronary sinus and its branches are preferred.
Q2: What is the Thebesian valve, and how does it affect coronary sinus cannulation?
A: The Thebesian valve is a thin membrane at the opening of the coronary sinus in the right atrium. It can partially or fully cover the ostium, making catheter and lead entry challenging or impossible without special techniques.
Q3: How does an AL2 catheter assist in coronary sinus cannulation?
A: The Amplatz Left 2 (AL2) catheter’s shape allows better alignment and stronger support against the atrial wall, helping to engage and cannulate the CS ostium even in the presence of an obstructive Thebesian valve.
Q4: Why use a hydrophilic Terumo wire?
A: The Terumo wire is flexible and smooth, making it easier to negotiate difficult or tortuous anatomy like fenestrations in the Thebesian valve without causing trauma.
Q5: What alternative pacing sites are used if right ventricular lead placement is not feasible?
A: Leads can be placed in the coronary sinus tributaries such as the posterolateral vein to achieve effective ventricular pacing without crossing the tricuspid valve.
Q6: What are the risks of placing leads across a bioprosthetic tricuspid valve?
A: Leads crossing the valve can impair valve function, increase the risk of valve damage or thrombosis, and potentially worsen heart failure symptoms.
Q7: Can preoperative imaging help in planning pacemaker implantation?
A: Yes, imaging like echocardiography or cardiac CT can provide valuable information about valve anatomy, CS ostium size, and Thebesian valve morphology to guide procedural strategy.
Q8: How common is complete heart block after tricuspid valve surgery?
A: It is an uncommon but well-recognized complication, occurring due to proximity of the conduction system to the tricuspid annulus and surgical manipulation.