A Detailed Case-Based Explanation
Abnormal heart rhythms (arrhythmias) can significantly affect quality of life and, in some cases, pose serious health risks. One such rhythm disorder is Focal Atrial Tachycardia (AT)—a condition where rapid heartbeats originate from a specific abnormal focus within the atria rather than the heart’s normal pacemaker.
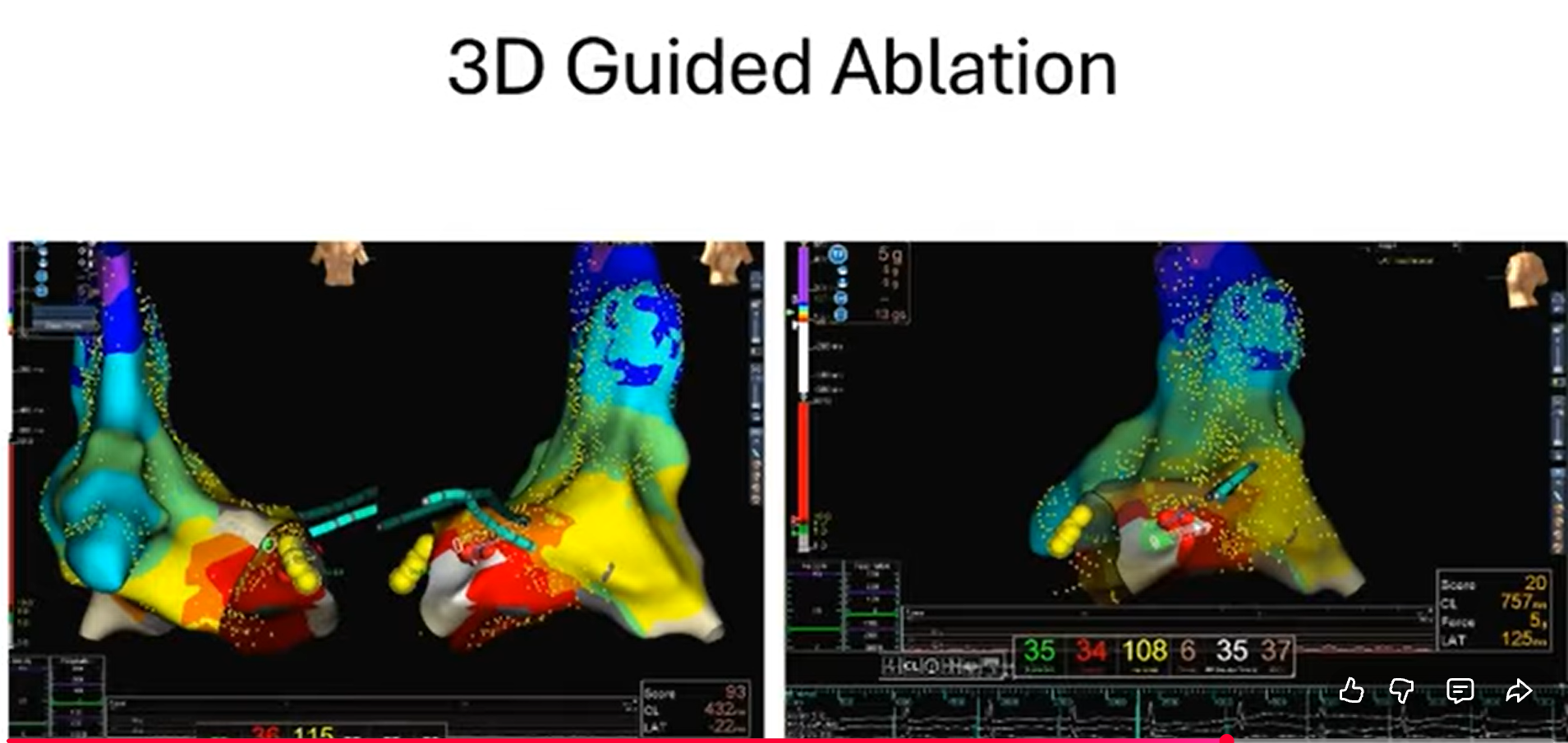
This blog presents a real-world electrophysiology case of focal atrial tachycardia, successfully treated using advanced 3D electroanatomical mapping and radiofrequency ablation (RFA) under expert care.
Understanding Focal Atrial Tachycardia
Focal atrial tachycardia is a form of supraventricular tachycardia (SVT) caused by an abnormal electrical focus in the atrium that fires independently of the sinus node. Unlike AVNRT or AVRT, atrial tachycardia often shows:
-
Long RP intervals
-
Variable P–P intervals
-
Poor response to conventional vagal maneuvers
-
Recurrence despite medications
Precise diagnosis is critical, as treatment strategies differ significantly.
Patient Presentation
-
Age / Gender: 58-year-old male
-
Medical History: Prior myocardial infarction (3 months earlier)
-
Symptoms:
-
Palpitations
-
Rapid pulse
-
Intermittent episodes of tachycardia
-
Baseline ECG Findings
Initial ECG revealed:
-
Narrow-complex tachycardia resembling PSVT
-
Long RP tachycardia
-
Inconsistent atrial cycle length
These findings raised suspicion of atrial tachycardia rather than AV nodal–dependent SVT, prompting an electrophysiology study (EPS).
Electrophysiology Study (EPS)
During the EP study:
-
Baseline ECG recorded prior to catheter placement
-
Decapolar and quadripolar catheters advanced into the right atrium via the inferior vena cava
-
Tachycardia was spontaneously induced
-
Entrainment attempts led to termination, supporting a non-reentrant mechanism
Tachycardia Induction
-
Atrial extrastimulus pacing performed from proximal decapolar electrodes
-
Drive train of 450 ms, followed by an extrastimulus at 260 ms
-
Sustained tachycardia successfully induced
-
Atrial activation sequence carefully analyzed
Confirming the Mechanism
To determine the exact mechanism:
-
Earliest atrial activation was seen in CS proximal electrodes
-
Ventricular Overdrive Pacing (VOP) demonstrated clear VA dissociation
-
This definitively confirmed focal atrial tachycardia
3D Electroanatomical Mapping
Advanced 3D mapping of the right atrium was performed during ongoing tachycardia:
-
Ventricular signals excluded using mapping windows
-
Activation and propagation maps created
-
Earliest atrial activation localized to the ostium of the coronary sinus (CS)
-
LAT mapping showed a focal earliest site correlating with CS-proximal electrograms
This step was crucial for accurate and safe ablation.
Radiofrequency Ablation (RFA)
-
Ablation catheter guided to the CS ostium
-
His bundle tagged to avoid AV conduction injury
-
RF energy delivered at a site showing 25 ms early atrial activation
-
Tachycardia terminated promptly
Post-Ablation Assessment
-
Patient monitored for 25 minutes post-ablation
-
Aggressive re-induction attempted:
-
With pacing
-
With and without isoprenaline
-
-
Tachycardia was non-inducible
-
Procedure concluded successfully with no complications
Clinical Outcome
✔ Successful elimination of focal atrial tachycardia
✔ No recurrence during post-ablation testing
✔ Demonstrates the effectiveness of 3D-guided RFA in complex atrial arrhythmias
Key Learning Points
-
Long RP tachycardia with variable P–P intervals → suspect atrial tachycardia
-
VA dissociation during VOP is diagnostic
-
CS-proximal earliest A suggests peri-CS focal AT
-
3D mapping improves precision and safety
-
His bundle tagging is essential when ablating near CS ostium
Doctor Profile
Dr. M. S. Chandramouli
Consultant Electrophysiologist
Dr. M. S. Chandramouli is a highly experienced electrophysiologist specializing in the diagnosis and catheter ablation of complex cardiac arrhythmias, including atrial fibrillation, atrial tachycardia, SVT, and ventricular arrhythmias.
He is known for:
-
Expertise in 3D electroanatomical mapping systems
-
High-success, low-complication ablation outcomes
-
Evidence-based, patient-centric arrhythmia care
📍 Practices at: Yashoda Hospitals Secunderabad
Frequently Asked Questions (FAQs)
1. What is focal atrial tachycardia?
It is a heart rhythm disorder where rapid heartbeats arise from a single abnormal focus in the atrium rather than the normal sinus node.
2. Is atrial tachycardia dangerous?
It can be benign in some patients but may cause symptoms, heart failure, or cardiomyopathy if persistent or untreated.
3. Can medications cure atrial tachycardia?
Medications may control symptoms but often fail to provide a permanent cure, especially in focal AT.
4. What is 3D mapping in electrophysiology?
3D mapping creates a detailed electrical map of the heart, helping identify the exact origin of abnormal rhythms with high precision.
5. Is radiofrequency ablation safe?
Yes. When performed by experienced electrophysiologists using 3D guidance, RFA is highly safe and effective.
6. What is the success rate of ablation for focal AT?
Success rates are typically 85–95%, depending on location and underlying heart disease.
7. How long does recovery take after ablation?
Most patients resume normal activities within 48–72 hours.
8. Will the arrhythmia come back?
Recurrence is uncommon but possible. Regular follow-up ensures early detection and management.
9. Do I need lifelong medication after ablation?
Many patients can discontinue anti-arrhythmic drugs after successful ablation, based on physician advice.
10. When should I see an electrophysiologist?
If you experience recurrent palpitations, unexplained fast heart rates, or medication-resistant arrhythmias, specialist evaluation is recommended.