Introduction
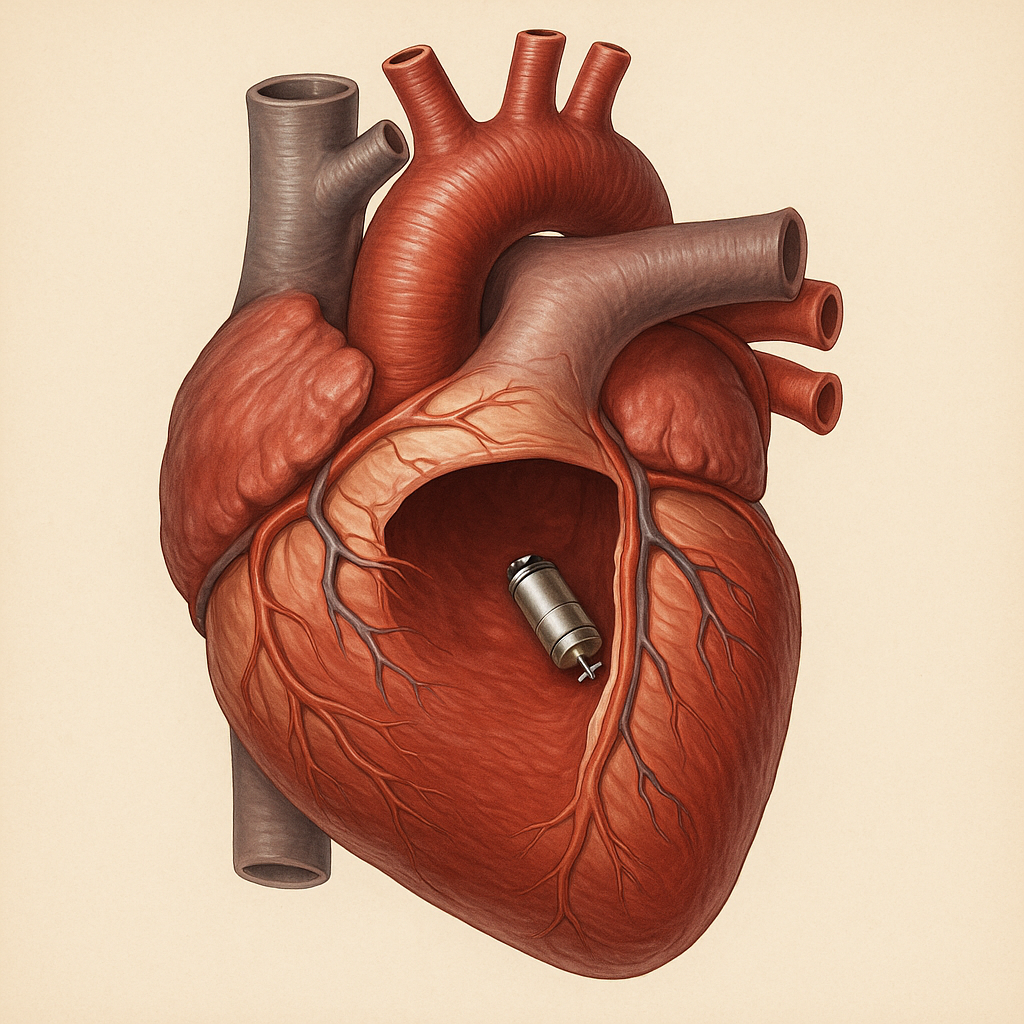
Imagine a tiny device, no bigger than a vitamin capsule, quietly nestled inside your heart, working tirelessly to keep your heartbeat steady—all without wires or a visible bump under your skin. Welcome to the era of leadless pacemakers, a breakthrough that is transforming the way we treat slow heart rhythms (bradycardia). In this 2,000-word deep dive, we’ll explore how these mini marvels work, their benefits, real-life stories, and practical considerations—finishing with a comprehensive FAQ to answer all your burning questions.
Table of Contents
1. The Journey to Leadless Technology
Pacemakers have been saving lives since the late 1950s. Early devices were bulky and required leads (insulated wires) threaded through veins into the heart. Over time, doctors encountered challenges:
-
Lead complications: fractures, dislodgement, infections
-
Pocket issues: infections or discomfort where the device sits under the skin
-
Aesthetic concerns: visible bulge on the chest
In response, engineers and electrophysiologists collaborated on miniaturizing pacemakers and eliminating leads altogether. The first commercially available leadless pacemaker was approved in 2016, marking a giant leap forward.
2. How Leadless Pacemakers Work
At its core, a leadless pacemaker is a self-contained, battery-powered capsule:
-
Size & Shape
-
About 25–30 mm long and 6–7 mm wide
-
Encased in biocompatible metal and polymers
-
-
Implantation Method
-
A catheter is inserted through the femoral vein in the groin
-
The device is guided into the right ventricle of the heart
-
Flexible tines anchor it to the heart muscle
-
-
Sensing & Pacing
-
Built-in electrodes sense intrinsic heartbeats
-
When a pause or slow rhythm is detected, the device delivers tiny electrical pulses
-
Pacing parameters can be programmed wirelessly by the physician
-
-
Power and Longevity
-
Battery life typically ranges from 8 to 15 years
-
Device transmits status during follow-up visits
-
3. Key Benefits
3.1 Minimally Invasive
-
No chest incision or subcutaneous pocket
-
Faster recovery, less scarring
3.2 Lower Infection Risk
-
Eliminates lead-related infections
-
Smaller vascular access site
3.3 Improved Patient Comfort
-
No visible device bump
-
Freedom from lead-related anxiety
3.4 Simplified Follow-Up
-
Remote monitoring capabilities
-
No leads to interrogate
3.5 MRI Compatibility
-
Modern designs are MRI-conditional, allowing many patients to safely undergo scans
4. Who’s a Candidate?
Leadless pacemakers aren’t a one-size-fits-all solution. Ideal candidates include:
-
Patients with single-chamber pacing needs (bradycardia affecting only the ventricles)
-
Individuals at high infection risk, such as those on dialysis or with prior device infections
-
Patients with limited venous access, e.g., after multiple prior leads have been placed
-
Active individuals concerned about lead fracture or dislodgement
A thorough evaluation by a cardiac electrophysiologist ensures the right device choice.
5. The Implantation Experience
Preparation
-
Local anesthesia and mild sedation
-
Anticoagulation management as needed
The Procedure (30–60 minutes)
-
Access: Femoral vein puncture under ultrasound guidance
-
Delivery: Catheter steered through the inferior vena cava into the right ventricle
-
Deployment: Device deployed and tines anchor to the heart wall
-
Testing: Sensing and pacing thresholds are verified
-
Closure: Vascular access site closed, pressure applied
Recovery
-
Observation for several hours to confirm hemostasis
-
Typically discharged the next day
-
Light activities within 48–72 hours; full recovery in 1–2 weeks
6. Living with a Leadless Pacemaker
Activity & Lifestyle
-
No heavy lifting or strenuous upper-body exercise for the first 2 weeks
-
Resume normal activities thereafter, including travel and exercise
-
Avoid strong electromagnetic fields (industrial equipment, high-power welding)
Device Checks
-
In-office device interrogation every 6–12 months, or via remote monitoring
-
Battery status, pacing thresholds, and sensing parameters reviewed
Travel & Security
-
Airport metal detectors do not affect the device
-
Inform security personnel; carry an ID card
7. Potential Risks and Limitations
-
Perforation Risk: Rare risk of heart wall perforation during implantation
-
Battery Depletion: When battery nears end-of-life, a new device is implanted; the old device may be left in place or retrieved if feasible
-
Single-Chamber Only: Not suitable for patients needing dual-chamber or biventricular pacing
-
Retrieval Complexity: Extraction of a chronically implanted device can be more challenging than lead removal
8. Future Innovations
The horizon is bright for leadless pacing:
-
Dual-Chamber Leadless Systems: Communicating right- and left-ventricular capsules for synchronized pacing
-
Enhanced Battery Technology: Longer life spans and potential for energy harvesting
-
Sensor Integration: Hemodynamic sensors to guide heart failure management
-
Mini-aturization: Even smaller devices for pediatric and structural heart applications
9. Patient Story: Rekha’s Leap of Faith
“I was terrified of having wires inside me,” recalls Rekha, a 68-year-old retired teacher diagnosed with slow heart rhythm after fainting spells.
The traditional pacemaker option meant a chest incision and visible bump. Lead complications worried her: “What if the wires break?”
Her electrophysiologist suggested a leadless pacemaker. Rekha was intrigued. On implantation day, she watched on a monitor as the tiny capsule floated through the catheter and snapped into place.
“I felt a flutter,” she laughs, recalling the moment the device took over pacing. Two days later, she walked out of the hospital free of chest scars. Six months on, Rekha swims daily and credits her “invisible guardian” for her renewed confidence.
10. FAQs
-
What exactly is a leadless pacemaker?
A leadless pacemaker is a self-contained device implanted directly inside the right ventricle, eliminating the need for wires (leads) and a subcutaneous pocket. -
How long does the implantation take?
The procedure typically lasts 30–60 minutes under local anesthesia and light sedation. -
Will I feel the device inside my heart?
No. Once secured, the device does not cause discomfort or awareness. -
How long will the battery last?
Most batteries last between 8 and 15 years, depending on pacing needs and device settings. -
What happens when the battery runs out?
A new device is implanted alongside or, if feasible, the old unit is retrieved. -
Can I have an MRI with this pacemaker?
Yes—modern leadless pacemakers are MRI-conditional. Always inform your imaging center about your device. -
Are there any activity restrictions?
Avoid strenuous upper-body exercise for 2 weeks post-implantation; thereafter, you can generally resume normal activities. -
What are common complications?
Rare risks include bleeding at the access site, heart wall perforation, or device dislodgement during the procedure. -
Who is not eligible for leadless pacing?
Patients needing dual-chamber pacing or cardiac resynchronization therapy are not candidates for current single-chamber leadless systems. -
How is follow-up managed?
Follow-up includes in-office visits every 6–12 months or remote monitoring via wireless data transmission. -
Is a leadless pacemaker visible on the chest?
No, since the device resides entirely within the heart, there’s no external bump. -
Do airport scanners affect my pacemaker?
No. The electromagnetic fields in standard security scanners are too low to interfere; however, carry your device ID card.